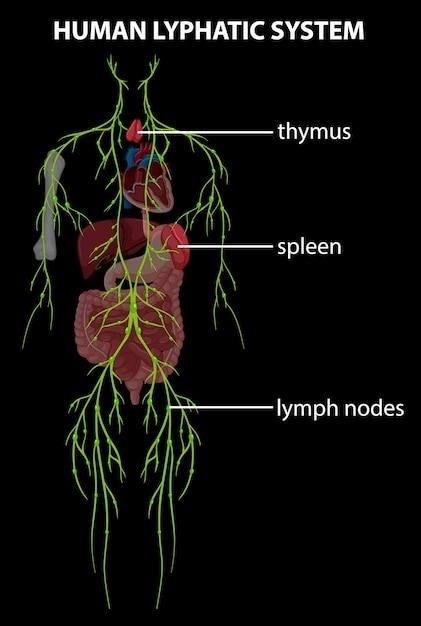
The Lymphatic System⁚ An Overview
The lymphatic system, a crucial component of the circulatory and immune systems, comprises a network of vessels, tissues, and organs. It maintains fluid balance, absorbs fats, and defends against pathogens, playing a vital role in overall health and well-being. Its intricate structure ensures efficient fluid transport and immune responses.
Fluid Balance and Recovery
The lymphatic system plays a pivotal role in maintaining the body’s fluid balance. As blood circulates, plasma leaks into tissues, forming interstitial fluid. This fluid contains vital nutrients and oxygen for cells. However, not all of this fluid is reabsorbed into the bloodstream; a significant portion remains in the tissues. The lymphatic system’s network of capillaries and vessels efficiently collects this excess interstitial fluid, preventing tissue swelling and edema. This collected fluid, now termed lymph, is then transported through increasingly larger lymphatic vessels towards the bloodstream. Lymph nodes, strategically positioned along these vessels, filter the lymph, removing waste products and pathogens before the fluid is returned to the circulatory system, completing the fluid balance cycle and maintaining tissue homeostasis. The efficient drainage of interstitial fluid is crucial for preventing fluid buildup and ensuring the proper functioning of cells and tissues throughout the body.
The Role of Lymphatic Vessels
Lymphatic vessels form an intricate network throughout the body, acting as conduits for the transport of lymph. Beginning as microscopic lymphatic capillaries, these vessels progressively increase in size, eventually culminating in larger lymphatic ducts that empty into the venous system near the heart. The lymphatic capillaries, with their unique one-way valves, efficiently collect interstitial fluid from tissues. These valves prevent the backflow of lymph, ensuring unidirectional movement towards the larger vessels. The larger lymphatic vessels, similar to veins, contain valves to maintain this directional flow. Smooth muscle contractions within the vessel walls and the pressure changes associated with breathing further facilitate lymph propulsion. This intricate system of vessels ensures the efficient collection and transport of lymph, contributing to both fluid balance and immune function. The structure and function of these vessels are crucial for maintaining overall health and preventing fluid accumulation.
Lymph Composition and Transportation
Lymph, the fluid transported within the lymphatic system, is a clear to yellowish liquid resembling plasma but with a lower protein concentration. Its composition includes water, dissolved proteins, fats, lymphocytes (a type of white blood cell crucial for immunity), and other immune cells. The lymphatic system’s primary function is to collect and filter this interstitial fluid from tissues, returning it to the bloodstream. This process is vital for maintaining fluid balance, preventing edema (swelling), and facilitating immune surveillance. Lymph is propelled through the lymphatic vessels by a combination of factors, including smooth muscle contractions within the vessel walls, skeletal muscle activity during movement, and pressure changes related to breathing. The unidirectional flow, maintained by valves within the vessels, ensures that lymph moves consistently towards the lymph nodes and ultimately back into the bloodstream via the thoracic duct and right lymphatic duct.
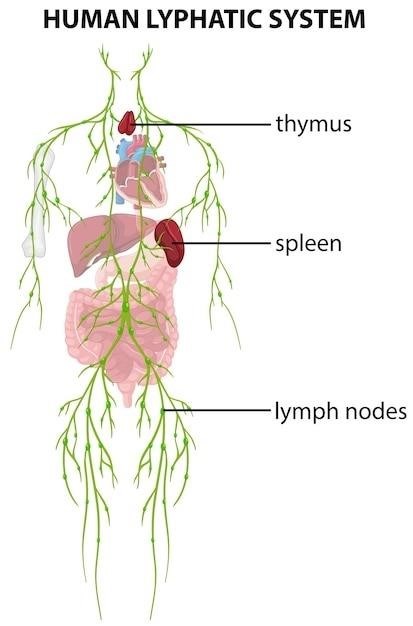
Key Lymphatic Structures and Organs
The lymphatic system includes lymph nodes, the spleen, the thymus, and tonsils—each playing a critical role in immune function and fluid balance, vital for overall health.
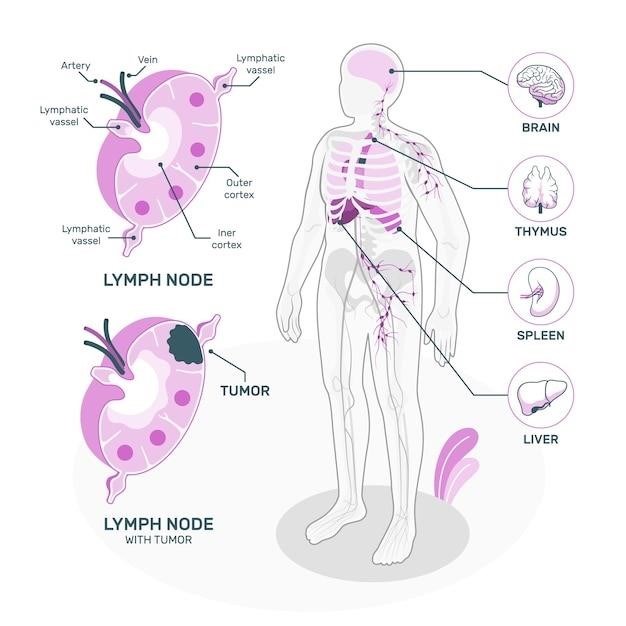
Lymph Nodes⁚ Structure and Function
Lymph nodes, small bean-shaped structures strategically located throughout the body, act as crucial filtration centers within the lymphatic system. These nodes are encased in a fibrous capsule and are composed of an outer cortex and an inner medulla. The cortex houses densely packed lymphocytes, including T cells and B cells, which are key players in the adaptive immune response. These lymphocytes continuously monitor the lymph for the presence of foreign antigens, such as bacteria, viruses, or other harmful substances.
When antigens are detected, the lymphocytes initiate an immune response, leading to the proliferation of specific immune cells and the production of antibodies. The medulla of the lymph node contains macrophages, phagocytic cells that engulf and destroy pathogens and cellular debris. The lymph nodes’ strategic positioning along lymphatic vessels ensures that lymph is thoroughly filtered before returning to the bloodstream, effectively preventing the spread of infection.
The size and activity of lymph nodes can vary depending on the state of the immune system. During infection, lymph nodes may become enlarged and tender due to increased lymphocyte activity and inflammation. This enlargement, often referred to as swollen glands, is a common sign of infection. The efficient filtration and immune surveillance provided by lymph nodes are essential for maintaining overall health and preventing the spread of disease.
The Spleen⁚ Immune Surveillance and Filtration
The spleen, the largest lymphoid organ in the body, plays a vital role in both immune function and blood filtration. Located in the upper left quadrant of the abdomen, it’s a highly vascular organ composed of two main regions⁚ red pulp and white pulp. The red pulp is primarily involved in filtering aged or damaged red blood cells from the circulation. These cells are phagocytosed by macrophages, removing them from the bloodstream and preventing their potential disruption of circulatory function. The spleen also acts as a reservoir for blood, releasing stored blood cells into circulation as needed.
The white pulp of the spleen, on the other hand, is crucial for immune surveillance. It contains a high concentration of lymphocytes, including T cells and B cells, which actively monitor the blood for the presence of foreign antigens. Upon encountering an antigen, these lymphocytes initiate an immune response, contributing to both humoral and cell-mediated immunity. This process helps protect the body from infection and disease. The spleen’s ability to filter blood and mount an immune response makes it an essential component of the body’s defense mechanisms.
In cases of splenic dysfunction or removal (splenectomy), the body’s ability to filter blood and fight infection can be compromised, potentially increasing susceptibility to certain infections. Therefore, the spleen’s role in both immune surveillance and blood filtration is crucial for maintaining overall health and well-being.
The Thymus⁚ T-Cell Maturation and Development
The thymus, a bilobed organ located in the mediastinum, plays a pivotal role in the development and maturation of T lymphocytes, crucial components of the adaptive immune system. Unlike other lymphoid organs, the thymus is most active during childhood and adolescence, gradually shrinking with age. Within the thymus, immature T cells, derived from bone marrow stem cells, undergo a complex process of differentiation and selection. This process ensures that only T cells capable of recognizing and responding to foreign antigens, while tolerating self-antigens, are allowed to mature and enter the circulation. Those T cells that fail to meet these stringent criteria undergo apoptosis, a programmed cell death mechanism, preventing autoimmunity. The thymus microenvironment, consisting of thymic epithelial cells and other specialized cells, is crucial for this maturation process.
The thymus secretes several hormones, including thymosin and thymopoietin, which influence T cell development and function. These hormones promote T cell proliferation, differentiation, and the expression of surface markers necessary for immune recognition. The thymus’s role in T cell maturation is therefore essential for establishing a robust and self-tolerant adaptive immune system, crucial for protecting against a wide range of pathogens and maintaining overall immune homeostasis. Thymic dysfunction can lead to immunodeficiency and increased susceptibility to infections.
Tonsils⁚ First Line of Defense
The tonsils, strategically located at the entrance of the pharynx, represent a crucial component of the body’s initial immune defense mechanism. These lymphoid aggregates, comprising the palatine, lingual, and pharyngeal tonsils (adenoids), are rich in lymphocytes and other immune cells. Their primary function is to intercept and neutralize pathogens, such as bacteria and viruses, that enter the body through the respiratory and digestive tracts. Upon encountering foreign antigens, the tonsils initiate an immune response, involving the activation of B cells and T cells, leading to the production of antibodies and the destruction of pathogens. This localized immune response helps prevent infection from spreading further into the body.
The tonsils’ anatomical location facilitates their role as a first line of defense, acting as a physical barrier and immunological surveillance point. While often associated with childhood infections, tonsillitis, the inflammation of the tonsils, highlights their active involvement in combating invading microorganisms. The tonsils’ immune function, while critical in early life, diminishes somewhat with age, but they remain important components of the overall immune system, contributing to the body’s defense against respiratory and oral pathogens. Their strategic placement at the entrance to the body’s major passageways ensures rapid detection and response to potential threats.
Lymphatic System and Immunity
The lymphatic system plays a pivotal role in the body’s immune response. It facilitates the circulation of lymphocytes and other immune cells, enabling them to effectively combat pathogens and maintain overall health.
Lymphocytes⁚ Key Players in Immune Response
Lymphocytes, a critical type of white blood cell, are the primary cellular components of the adaptive immune system. These cells are produced and mature in the primary lymphoid organs, including the bone marrow and thymus. There are two main types of lymphocytes⁚ B cells and T cells. B cells are responsible for producing antibodies, which are specialized proteins that bind to specific antigens (foreign substances) and neutralize them. This antibody-mediated immunity is crucial for eliminating extracellular pathogens. T cells, on the other hand, directly attack infected cells or cancer cells, or they help regulate the immune response by interacting with other immune cells. The various subsets of T cells, including helper T cells, cytotoxic T cells, and regulatory T cells, work together in a coordinated manner to eliminate pathogens and maintain immune homeostasis. The intricate interplay between these lymphocyte types ensures a robust and specific immune response to a wide range of threats. The lymphatic system provides the structural framework for lymphocyte trafficking and interactions, facilitating their efficient mobilization throughout the body.
Macrophages⁚ Phagocytosis and Antigen Presentation
Macrophages, large phagocytic cells derived from monocytes, are essential components of the innate immune system. Residing in various tissues, they act as the body’s first line of defense against invading pathogens. Their primary function is phagocytosis—engulfing and destroying foreign particles, including bacteria, viruses, and cellular debris; This process is crucial for eliminating pathogens and preventing infection. Beyond phagocytosis, macrophages play a vital role in antigen presentation. After engulfing a pathogen, macrophages process and present fragments of its antigens on their surface via Major Histocompatibility Complex (MHC) molecules. This presentation is critical for activating T cells, a key component of the adaptive immune response. By presenting antigens, macrophages bridge the innate and adaptive immune systems, ensuring a coordinated and efficient immune response. Their strategic locations within tissues, including the lymphatic system, ensures quick responses to local infections.
The Interplay Between Lymphatic and Immune Systems
The lymphatic and immune systems are intricately linked, working in concert to maintain the body’s defense against pathogens. The lymphatic system provides the infrastructure for immune cell trafficking, transporting lymphocytes and other immune cells throughout the body. Lymph nodes, strategically located along lymphatic vessels, serve as filtering stations and sites of immune cell activation. Antigens, captured by macrophages and dendritic cells within the lymphatic system, are presented to T and B lymphocytes, initiating the adaptive immune response. Lymphocytes, produced in primary lymphoid organs like the bone marrow and thymus, circulate through the lymphatic system, encountering antigens and initiating immune responses. The spleen, a key lymphatic organ, filters blood, removing pathogens and damaged cells, contributing to both innate and adaptive immunity. This close collaboration ensures a rapid and effective response to infections, preventing disease and maintaining overall health. The efficient transport of immune cells and antigens through the lymphatic network underpins a robust and coordinated immune response.
Clinical Significance of the Lymphatic System
Dysfunction within the lymphatic system can lead to serious health issues, including lymphedema and immune deficiencies. Understanding its role is crucial for diagnosing and treating various diseases.
Lymphedema⁚ Causes and Treatment
Lymphedema, a debilitating condition, arises from impaired lymphatic drainage, leading to fluid accumulation and tissue swelling. Primary lymphedema stems from congenital lymphatic system abnormalities, while secondary lymphedema results from acquired damage, often due to cancer treatments (like lymph node removal or radiation therapy), infections (like filariasis), or injuries. The severity varies, ranging from mild swelling to significant limb enlargement, causing discomfort, pain, and increased risk of infection. Effective management involves a multi-faceted approach, including Complete Decongestive Therapy (CDT). CDT integrates manual lymphatic drainage massage, compression bandaging, exercises to stimulate lymphatic flow, and meticulous skin care to prevent infection. Other treatments include pneumatic compression pumps, medication to reduce inflammation, and in severe cases, surgical interventions might be considered. Early diagnosis and intervention are key to optimal outcomes, improving quality of life and minimizing long-term complications associated with this chronic condition. Patient education on self-care and adherence to the prescribed treatment plan are essential for successful management.
Autoimmune Diseases and Lymphatic Dysfunction
The intricate relationship between the lymphatic system and the immune system highlights its significant role in autoimmune diseases. These diseases arise from the immune system mistakenly attacking the body’s own tissues. Lymphatic dysfunction can contribute to or exacerbate autoimmune conditions. For instance, impaired lymphatic drainage might lead to the accumulation of immune complexes, potentially triggering or worsening inflammation in target organs. Conversely, dysregulation of immune cells within the lymphatic system could contribute to the development of autoimmunity. Conditions like rheumatoid arthritis, systemic lupus erythematosus, and multiple sclerosis have been associated with lymphatic abnormalities. Research is ongoing to explore the specific mechanisms linking lymphatic dysfunction and autoimmune diseases. Understanding these connections is crucial for developing targeted therapies that address both the immune response and lymphatic drainage to effectively manage autoimmune conditions and improve patient outcomes. Further research promises to unravel the intricate interplay between these systems.
Research and Future Directions
Ongoing research into the lymphatic system focuses on several key areas. A deeper understanding of lymphatic vessel development and the complex interactions between lymphatic endothelial cells and immune cells is crucial. Advanced imaging techniques are improving our ability to visualize and analyze lymphatic function in vivo, providing valuable insights into disease processes. Investigating the role of the lymphatic system in cancer metastasis is a major focus, aiming to identify novel therapeutic targets and improve cancer treatment strategies. The lymphatic system’s involvement in various inflammatory and autoimmune diseases is also under intense scrutiny. Studies are exploring the potential of lymphatic-targeted therapies to treat these conditions. Future research will likely leverage advanced technologies such as single-cell genomics and bioinformatics to comprehensively map the cellular composition and functional heterogeneity of the lymphatic system. This will undoubtedly lead to a more precise understanding of its role in health and disease, paving the way for the development of innovative diagnostic tools and therapeutic interventions.